Unraveling Oropharyngeal Dysphagia in Dementia: A Vital Understanding
Oropharyngeal dysphagia (OD) is increasingly recognized as a critical aspect affecting geriatric health, with particularly severe implications in patients suffering from dementia. As our population ages, understanding the intersections of dysphagia and neurodegenerative diseases becomes not just a clinical need but also a societal imperative. This article aims to provide insights into the endoscopic characterization of OD in dementia patients, highlighting the importance of proper diagnosis and tailored interventions.
The Complications of Dysphagia in Dementia
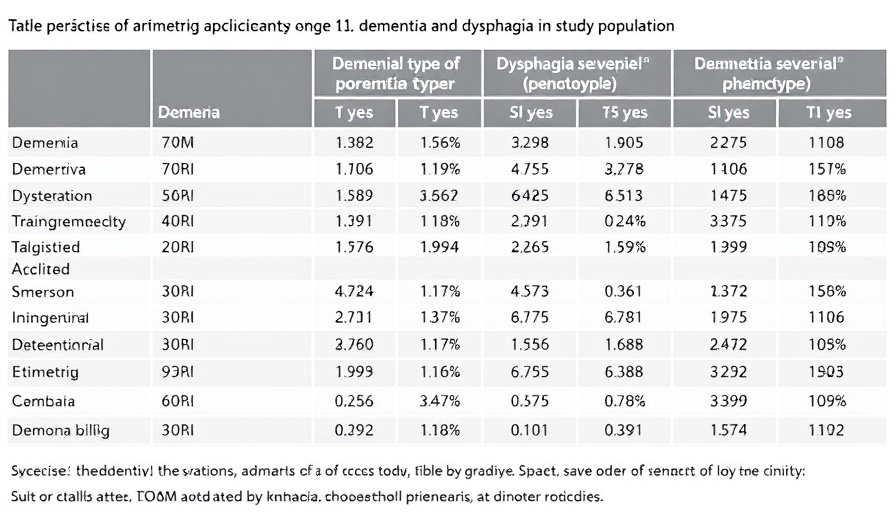
Dysphagia is more than just difficulty swallowing; it poses significant risks such as malnutrition, dehydration, aspiration pneumonia, and even increased mortality in older adults. The prevalence of dysphagia in dementia patients is higher than in the general population, yet research focusing on dysphagia's manifestation within various types of dementia remains limited. The 2025 study involving 107 hospitalized geriatric patients offers much-needed clarity, revealing that while there are shared characteristics across dementia types, unique patterns emerge, particularly among patients with Parkinson’s-related dementia.
Understanding the Research: Methodology and Findings
The retrospective analysis deployed a standardized Flexible Endoscopic Evaluation of Swallowing (FEES) protocol to systematically assess 107 patients diagnosed with Alzheimer’s dementia, mixed dementia, and Parkinson’s syndrome dementia. Key findings indicate that bolus residue occurred throughout the dementia spectrum; however, penetration and complex dysphagia, defined as the presence of two dysphagia indicators, were markedly higher among Parkinson's patients. This underscores the necessity for tailored dysphagia assessments and treatments to improve patient outcomes.
Telomeres and the Aging Process: A Biological Insight
The connection between aging and telomere biology offers a fascinating lens through which we can understand the complexities of health in older populations. Telomeres, the protective caps on chromosome ends, play a crucial role in cellular aging and function. Research has shown that as we age, telomeres shorten, leading to diminished cell function and an increased risk of age-related diseases, including neurodegenerative disorders like dementia. Enhancing telomerase activation and preserving telomere length through lifestyle choices and potential supplements may someday play a pivotal role in mitigating dysphagia and other geriatric syndromes.
Actionable Insights: Improving Outcomes for Patients with Dementia
To significantly enhance care for dementia patients experiencing dysphagia, the healthcare community can implement several actionable insights:
- Conduct regular endoscopic assessments to provide precise characterizations of dysphagia.
- Tailor nutrition plans that account for individual swallowing capabilities to ensure adequate hydration and nutrient intake.
- Explore the role of telomere health in dementia management, promoting lifestyle interventions that may slow telomere shortening, such as stress reduction, anti-inflammatory diets, and regular physical activity.
Future Directions: Implications for Research and Care
Given the aging global population, ongoing research is critical to understanding the dynamics between dysphagia and dementia. Future studies could explore the efficacy of telomere-targeted therapies in enhancing overall health and potentially easing dysphagia symptoms. Furthermore, continued advancements in endoscopic techniques could refine our capabilities in diagnosing and treating swallowing disorders.
Conclusion: The Path Forward
As our understanding of dysphagia in dementia deepens, so too does the responsibility of both healthcare providers and caregivers to advocate for appropriate care and interventions. By forging connections between ongoing research, such as telomere studies, and practical applications in clinical settings, we can pave the way not only for improved outcomes in dysphagia management but also for enhanced overall quality of life in our aging population.
 Add Row
Add Row  Add
Add 




Write A Comment