
Understanding Refractive Error in Glaucoma Surgery
Refractive errors are common complications after surgical procedures such as phacoemulsification combined with intraocular lens implantation, particularly in patients with primary angle-closure glaucoma (PACG). This condition not only affects vision but can also be a marker of underlying cellular health dynamics. Research indicates that these errors might stem from various biometric parameters, which include the patient’s age, ocular biometry, and surgical techniques employed during the operation.
Linking Cellular Health to Surgical Outcomes
The connection between cellular rejuvenation and surgical outcomes cannot be overstated. Age, a significant factor in both glaucoma and refractive errors, is closely linked to cellular senescence—that is, the gradual decline in cellular function that affects regeneration and repair processes. As we age, our cells exhibit reduced mitochondrial function and inefficient cellular repair mechanisms. This decline impacts surgical recovery, which is why understanding how cellular health may influence outcomes is pivotal for optimizing surgical strategies.
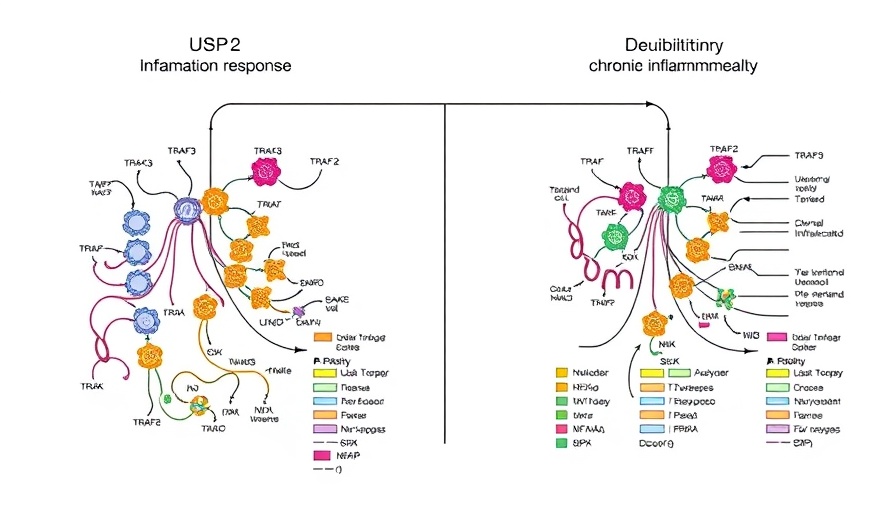
A Multifactorial Approach to Minimizing Risk
In dealing with the intricate interplay of surgical techniques and biological variability, doctors are now emphasizing a multifactorial approach. This includes assessing patient history, anatomical metrics, and cellular indicators. For instance, studies have shown that patients exhibiting better mitochondrial function—often influenced by factors such as diet and nutritional supplementation—tend to recover more efficiently from surgeries like phacoemulsification. Incorporating potential NAD+ boosters or exploring stem cell therapies as preoperative measures could enhance cellular repair and ultimately improve surgical outcomes.
Future Trends: Personalized Medicine and Regenerative Therapies
The future of treating refractive errors post-surgery may lie in personalized medicine, where treatments are tailored based upon an individual's unique cellular makeup and biological markers. Innovations in regenerative medicine are also pivotal; for example, therapies that enhance autophagy could clear out damaged cellular components, rejuvenating the cells necessary for healing. Maintaining cellular health through lifestyle choices, such as balanced diets rich in antioxidants, may provide significant advantages in recovery. This knowledge positions patients as active participants in their health outcomes, encouraging them to consider their cellular and mitochondrial health as integral to their surgical journey.
Take Charge of Your Cellular Health
Understanding the connection between cellular function and surgical outcomes can empower individuals to make lifestyle changes that pave the way for improved health. For those undergoing eye surgery, investigating anti-aging cellular strategies, such as enhanced mitochondrial function through dietary interventions and considering regenerative medicine, may streamline recovery and reduce complications. By prioritizing cellular rejuvenation, patients not only prepare their bodies for surgery but also foster long-term vitality.
For those interested in diving deeper into cellular health, consider consulting with professionals in regenerative medicine or nutrition, who can guide you through practical steps toward rejuvenation.
 Add Row
Add Row  Add
Add 


Write A Comment